 Little did I know, back in 2017 when I started this blog – and this particular series – that I would end up writing a ‘Part 5‘…nor did I know that my journey to an ‘electric brain‘ wasn’t complete yet. I would never have dreamed in a million years that I would, once again go under the ‘knife‘, so to speak, with an additional DBS surgery to have an extra lead inserted! “Nope, nope, no way; I ain’t never going through the ordeal of more brain surgery, and especially having that ‘Halo’ thingy screwed into my skull again!!” Well, I guess I should have taken my own advice that I gave to y’all and remember to “Never Say Never“!! And so, in May 2021 (as I mentioned at the end of my posting ‘‘My Life, Updated’ for Parkinson’s Awareness Month 2021‘), I went into surgery once again to have a new GPi ‘rescue‘ wire installed.
Little did I know, back in 2017 when I started this blog – and this particular series – that I would end up writing a ‘Part 5‘…nor did I know that my journey to an ‘electric brain‘ wasn’t complete yet. I would never have dreamed in a million years that I would, once again go under the ‘knife‘, so to speak, with an additional DBS surgery to have an extra lead inserted! “Nope, nope, no way; I ain’t never going through the ordeal of more brain surgery, and especially having that ‘Halo’ thingy screwed into my skull again!!” Well, I guess I should have taken my own advice that I gave to y’all and remember to “Never Say Never“!! And so, in May 2021 (as I mentioned at the end of my posting ‘‘My Life, Updated’ for Parkinson’s Awareness Month 2021‘), I went into surgery once again to have a new GPi ‘rescue‘ wire installed. “Whoa! Now wait a minute, Tom… MAY of 2021? That’s almost a year and a half ago! Why did you wait so long to tell us about the results of this?” Well…. that’s a very good question. And I will tell you why… later in this posting. There’s a reason for my insanity, and I think you’ll see why I HAD to wait until now to tell you my story. But before I can fully begin this “tale of mystery“… we need to learn a few things about the GPi – what it is, what it does, and why they use it in DBS. So, kiddies, it’s time we put our ‘Learning‘ caps back on, and go back to “Brain 101” class!
“Whoa! Now wait a minute, Tom… MAY of 2021? That’s almost a year and a half ago! Why did you wait so long to tell us about the results of this?” Well…. that’s a very good question. And I will tell you why… later in this posting. There’s a reason for my insanity, and I think you’ll see why I HAD to wait until now to tell you my story. But before I can fully begin this “tale of mystery“… we need to learn a few things about the GPi – what it is, what it does, and why they use it in DBS. So, kiddies, it’s time we put our ‘Learning‘ caps back on, and go back to “Brain 101” class!
![]() R-I-N-G
R-I-N-G ![]()
OK, class is now in session!
[Note: If you really feel you know everything there is to know about the GPi, you can take this one-time free ‘SKIP THE FIRST HALF OF CLASS” card and proceed to the ‘DBS and the GPi‘ section. But no cheating now!]
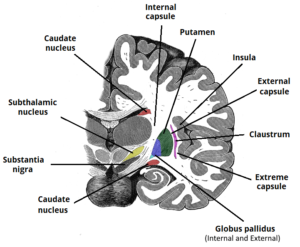
THE BASAL GANGLIA
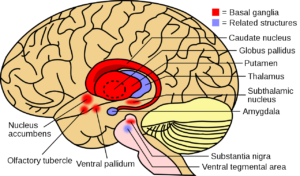 So, what exactly is this GPi, or Globus Pallidus Internus? The GPi is located deep inside the brain in whats called the subcortical structure. It, along with the Globus Pallidus Externus (GPe), make up the full Globus Pallidus (GP). And that, along with a few other structures – including our familiar Subthalamic Nucleus (STN) and Substantia Nigra (SN), make up the entire Basal Ganglia (BG) (which I’m sure you’ve heard me talk about before).
So, what exactly is this GPi, or Globus Pallidus Internus? The GPi is located deep inside the brain in whats called the subcortical structure. It, along with the Globus Pallidus Externus (GPe), make up the full Globus Pallidus (GP). And that, along with a few other structures – including our familiar Subthalamic Nucleus (STN) and Substantia Nigra (SN), make up the entire Basal Ganglia (BG) (which I’m sure you’ve heard me talk about before).
Now, the Basal Ganglia area is assigned a LOT of brain duties, such as: Control of voluntary motor movements, procedural and habit learning, conditional learning, eye movements, cognition, and emotion. I see a hand go up in the back of the class… Yes, miss? “Hey, you said motor movements! Isn’t that the problem that occurs with Parkinson’s?” Yes ma’am, you are correct, and you get my first star of the day! Parkinson’s Disease begins in the Substantia Nigra with the gradual loss of the cells that produce the neurotransmitter dopamine. The Basil Ganglia and other parts of the brain, use that dopamine to help with movement, both voluntary and involuntary. When those dopamine cells in the SN die, less and less dopamine is produced for the GP to use for smooth movement, and that results in the patient experiencing their first motor symptom(s) of Parkinson’s Disease.
BACK TO THE GPi
 Whew! Talk about a lot of long medical terms, huh? Trust me, that was a very basic discussion of the parts involved. (And if that wasn’t enough for you, then you can learn more by googling something like ‘Parkinson’s Disease and GPi’) Not to worry, though, I’ll try to simplify it a bit as we now go back to the GPi.
Whew! Talk about a lot of long medical terms, huh? Trust me, that was a very basic discussion of the parts involved. (And if that wasn’t enough for you, then you can learn more by googling something like ‘Parkinson’s Disease and GPi’) Not to worry, though, I’ll try to simplify it a bit as we now go back to the GPi.
As I said before, the entire GP itself is used, along with the dopamine from the STN, to help regulate smooth and controlled movements in the body. Say, for instance, when someone begins to engage in an activity such as petting a dog, for example; these structures help regulate the movement to make it as smooth as possible, and to respond to sensory feedback. Both the GP and STN are involved in the constant subtle regulation of movement that allows people to walk and engage in a wide variety of other activities with a minimal level of disruption. I like to think they act kinda like a ‘pacemaker‘ of movement.
However, when the function of the GP is affected, such as low or no dopamine from the STN, Parkinson’s movement disorders begin occurring, such as: Tremors, dystonia, walking problems, jerky movements, etc.
 DBS and the GPi
DBS and the GPi
Now that we know a little bit more about the GPi, our final discussion in this class will be about DBS and the GPi. We know that, for whatever reason, putting electrical stimulation (DBS) into a receiving area of the brain, can change the behavior of that area. One theory is that it somehow ‘smooths‘ out the electrical area where movement signals become mixed up and produce PD symptoms. For Parkinson’s, several stimulation targets have been identified over the last 20 years, but the two that have emerged as the most viable for treating the cardinal symptoms of PD are the STN and GPi. Although they are somewhat alike in that they assist in physical movement, there are differences. Physically, size is the most obvious difference between the GPi and STN. I’m told that the STN is about the size of a grain of rice (approximately 150mm). However, the GPi is a much larger target (approximately 450mm). Because the GPi is larger than the STN, the average electric charge required for effective stimulation of that area tends to be higher than for the STN. So by having a GPi implant, one could anticipate more battery use and drainage, which means more battery changes (this can be remedied by using a rechargeable battery).
Normally, for Parkinson’s DBS, neurologists almost always recommend starting with the STN, for various reasons (which we’ll discuss in a moment). In fact, as you know, my first DBS in 2017 was in the STN… Heck, I hadn’t even heard of a ‘GPi‘ region until probably late 2020! But it turns out that DBS of the GPi is also an established, safe and effective method for addressing many of the motor symptoms associated with PD. This includes: bradykinesia, rigidity, and tremor control. GPi DBS also has an important advantage: a Direct anti-dyskinetic effect. And I’m told it is actually easier to program in the outpatient setting. But the BIG, MOST IMPORTANT reason that I opted for GPi DBS was that it has been shown to have a direct effect on… you got it, DYSTONIA!
Ah ha, now I got your attention, huh? After we had tried almost everything – and I mean everything – we could do with the STN lead, I opted to go under the knife again with the hope that having this GPi ‘rescue wire‘ would FINALLY rid me of Ms. Dystonia’s torture for good!
 I must have become a mind reader of sort, because I know what next question will be… Yes? The young man on the right in the red sweater… “Wow, Tom, that sounds good! Maybe you should have done GPi DBS instead of the STN right at the start in 2017!” That’s what I thought too when I first researched the GPi; and a lot of researchers think that same thing; however the choice between selection of the STN or GPi really depends on the patient; it should be discussed and used by each patient individually based on their need. In some cases, like mine, it may be better to have BOTH. In my case, there is one VERY IMPORTANT difference that stands out between DBS in the STN vs. the GPi areas:
I must have become a mind reader of sort, because I know what next question will be… Yes? The young man on the right in the red sweater… “Wow, Tom, that sounds good! Maybe you should have done GPi DBS instead of the STN right at the start in 2017!” That’s what I thought too when I first researched the GPi; and a lot of researchers think that same thing; however the choice between selection of the STN or GPi really depends on the patient; it should be discussed and used by each patient individually based on their need. In some cases, like mine, it may be better to have BOTH. In my case, there is one VERY IMPORTANT difference that stands out between DBS in the STN vs. the GPi areas:
In the STN, once that lead is turned on at the first programming session, it produces an immediate effect – Tremors lessen or go away, rigidity is much less, etc. That’s one of the reasons I was awake during my STN surgery in 2017 – in the OR, they turned the probe on for a short time once it was in place, and I could feel my muscles and toes begin to relax; I don’t have any tremor, but I’ve heard – and seen – that once it’s turned on, the tremor almost always goes away or lessens immediately.
Not so with the GPi, especially when dystonia is involved. You see, the BIG difference between DBS in the more-common STN vs. the GPi, is this: The GPi TAKES TIME for the stimulation to become effective! Turning on a GPi lead for the first time most likely results in the patient not seeing any improvement at that point.
 Now I see a bunch of light bulbs going off in class, hands shooting up everywhere! You, the freckle faced kid in the back row, yes? “I know, I know, that’s why you had to wait to tell us about your surgery til now; it took time for your new implant to ‘TAKE’… Right? Right?” You, sir, are correct – give him a big old gold star! I was told, on average, it might take MONTHS of increasing stimulation for it to have an effect on the dystonia – hence I decided “Why write about something when I can’t tell if it’s even working yet?” It could be 3 months, 6 months, or even a couple of years before the GPi DBS would hopefully drive old Ms. Dystonia out of my head! And the funny thing is… no one has told me exactly WHY it takes so long to become effective…. maybe because of the size difference between the STN and GPi? Or some kind of other mystical property?? Maybe no one really knows, but in any case I felt it was worth the chance to finally rid myself of this accursed toe cramping!
Now I see a bunch of light bulbs going off in class, hands shooting up everywhere! You, the freckle faced kid in the back row, yes? “I know, I know, that’s why you had to wait to tell us about your surgery til now; it took time for your new implant to ‘TAKE’… Right? Right?” You, sir, are correct – give him a big old gold star! I was told, on average, it might take MONTHS of increasing stimulation for it to have an effect on the dystonia – hence I decided “Why write about something when I can’t tell if it’s even working yet?” It could be 3 months, 6 months, or even a couple of years before the GPi DBS would hopefully drive old Ms. Dystonia out of my head! And the funny thing is… no one has told me exactly WHY it takes so long to become effective…. maybe because of the size difference between the STN and GPi? Or some kind of other mystical property?? Maybe no one really knows, but in any case I felt it was worth the chance to finally rid myself of this accursed toe cramping!
Well, I see it’s almost 4pm – time for this class to end. But before we leave today, here for your review is a summary comparison between STN and GPi DBS methods:
STN DBS
GPi DBS
 OK y’all have been GREAT students today! So without further ado….
OK y’all have been GREAT students today! So without further ado….
![]() R-I-N-G
R-I-N-G ![]() , Class DISMISSED!!
, Class DISMISSED!!
Hold it…not the rest of you! Stay here, please… Although long-winded, I hope that gave you a bit of knowledge about the GPi and why I waited till now to write this. So, with that, let’s go back to the beginning for REAL story!

Well, as I mentioned at the beginning, the story continues from the end of my previous post “‘My Life, Updated’ for Parkinson’s Awareness Month 2021“. The very next day I was back at the hospital at 5am for my GPi procedure. Now mind you – this was my second time around for brain surgery, and although I couldn’t say I was an old ‘pro‘ at it, I at least felt I knew what to expect.
 Or at least I thought…. Anyway, after arriving at the hospital and checking in, I went through the same old routine and prep as before. Just before they took me into the OR, I was taken once again into a separate room with the nurse to finalize the prep. That’s when I heard that sound, and it filled me with a horrible dread! The pitter-patter of hospital shoes, along with an ominous clinking of steel on steel. And that’s when he appeared: My surgeon’s torture boy (i.e. his PA) carrying that hideous HALO in his hands! Ugh… well, I did it once so I guess I can do it again… At least now I know what to expect, right? Right…. EXCEPT this time, while attaching (i.e. screwing the thing into my skull) the back right side of the halo, he must has hit a nerve directly, because – and I say this mildly – I was hit with a pain that felt like a hot iron was poking into my skull!! This pain lasted around 45-60 seconds, during which time I groaned, moaned, and -almost- announced I was ending the whole procedure by saying, “ARGH! Take it off! Forget the whole thing! I can’t stand the pain anymore!” But thankfully, after numerous injections of pain killer to that one area, the pain finally calmed down… Though it still, as always, felt like my head was in a vise – but at least that hideous pain was gone!! Whew!
Or at least I thought…. Anyway, after arriving at the hospital and checking in, I went through the same old routine and prep as before. Just before they took me into the OR, I was taken once again into a separate room with the nurse to finalize the prep. That’s when I heard that sound, and it filled me with a horrible dread! The pitter-patter of hospital shoes, along with an ominous clinking of steel on steel. And that’s when he appeared: My surgeon’s torture boy (i.e. his PA) carrying that hideous HALO in his hands! Ugh… well, I did it once so I guess I can do it again… At least now I know what to expect, right? Right…. EXCEPT this time, while attaching (i.e. screwing the thing into my skull) the back right side of the halo, he must has hit a nerve directly, because – and I say this mildly – I was hit with a pain that felt like a hot iron was poking into my skull!! This pain lasted around 45-60 seconds, during which time I groaned, moaned, and -almost- announced I was ending the whole procedure by saying, “ARGH! Take it off! Forget the whole thing! I can’t stand the pain anymore!” But thankfully, after numerous injections of pain killer to that one area, the pain finally calmed down… Though it still, as always, felt like my head was in a vise – but at least that hideous pain was gone!! Whew!
 After the halo was attached and secured, once again I was wheeled into the OR, complete with the OR crew and the same kind of equipment and whirring sound of machines as I had in 2017. They got me on the table and began locking that halo – with my head in it – into the frame directly behind me. Here, though, is where it gets different from before: Last time, I was fully awake during everything except the drilling. However, this time… I was looking around, talking to people, answering and asking questions – then somehow my surgeon must has made a hand signal or something to the anesthesiologist, because in mid-sentence – WHAM! I blinked… and the next thing I remember after opening my eyes, was that the room seemed darker than it was just a second before, and very quiet. Standing in front of me was my Boston Scientific rep; in his hand was a control unit with a wire stretching from it to somewhere behind me. He said, “OK Tom, we have the probe into your GPi and now we want to see if there are any side effects.” WHAT? Really? Already? Unlike my STN surgery, I remember nothing. Why? Remember, the STN produces an immediate effect when turned on, even in the OR; whereas with the GPi it’s delayed. Since I most likely wasn’t going to notice any improvement or effect, why should I be awake the entire surgery?
After the halo was attached and secured, once again I was wheeled into the OR, complete with the OR crew and the same kind of equipment and whirring sound of machines as I had in 2017. They got me on the table and began locking that halo – with my head in it – into the frame directly behind me. Here, though, is where it gets different from before: Last time, I was fully awake during everything except the drilling. However, this time… I was looking around, talking to people, answering and asking questions – then somehow my surgeon must has made a hand signal or something to the anesthesiologist, because in mid-sentence – WHAM! I blinked… and the next thing I remember after opening my eyes, was that the room seemed darker than it was just a second before, and very quiet. Standing in front of me was my Boston Scientific rep; in his hand was a control unit with a wire stretching from it to somewhere behind me. He said, “OK Tom, we have the probe into your GPi and now we want to see if there are any side effects.” WHAT? Really? Already? Unlike my STN surgery, I remember nothing. Why? Remember, the STN produces an immediate effect when turned on, even in the OR; whereas with the GPi it’s delayed. Since I most likely wasn’t going to notice any improvement or effect, why should I be awake the entire surgery?
But the main reason they woke me up once the probe was in place, was to make sure that energizing that wire wouldn’t affect me in some other way (the lead does pass close to the optic nerve). Once he verified that I had no side-effects with the current on, someone must have once again done the ‘secret signal‘, because the next thing I knew they were done, the halo had been removed (thank goodness), and they were preparing to send back to my room for the night! Well, I guess that was a little easier than the 2017 STN surgery… except for that blasted halo! Anyway, once back in my room, I felt much more fatigued than I did after the first surgery, so after visiting with my wife and family a bit (and getting some breakfast – I was famished!), I slept for pretty much the remainder of the day. Everything proceeded then just like before (except for a 6pm heated argument with a ‘By the book, Just graduated’ evening nurse over dosage and timing of my meds! Don’t worry, I won!)
Side Note: However, I did hear later that day about something that went on during my surgery. Turns out my dear departed Dad was right in calling me a ‘hard head’ at times… Apparently, my surgeon tried a number of times to drill into my skull at his first choice location… Couldn’t drill through my hard head! So he ended up (successfully, but I’m sure with a few choice words) drilling into a slightly different but adjacent area.
Boy, Dad, you were right again! No wonder I have a hard time getting things into my brain!

After this, I went home and began to heal. Two weeks later I came in to have my second battery unit installed into my right chest. Yes folks, I now have two big bumps – one on each side – of my chest! The reason why is that the first one was done in 2017 with the old style, four-contact Medtronic leads. They are basically now an ‘older‘ technology, in that the electrical field can be moved up and down, and increased/decreased, but that was basically it.
 Now, however, I have a new top-of-the-line Boston Scientific Vercise Genus system with the Cartesia™ Directional lead and accompanying battery!! I’ll let you research their systems yourself, but in a nutshell these leads have more contacts, and are completely directional – the stimulation can be moved around any area of the contact; which not only helps deliver stimulation with pin-point accuracy, but can also help avoid side effects. In addition, the battery is fully rechargeable and good for 15+ years!
Now, however, I have a new top-of-the-line Boston Scientific Vercise Genus system with the Cartesia™ Directional lead and accompanying battery!! I’ll let you research their systems yourself, but in a nutshell these leads have more contacts, and are completely directional – the stimulation can be moved around any area of the contact; which not only helps deliver stimulation with pin-point accuracy, but can also help avoid side effects. In addition, the battery is fully rechargeable and good for 15+ years!
So, after a few more weeks of healing, I went back to my neurologist (along with my favorite Boston rep) and had the new GPi wire turned on and programmed for the first time!! And the result?!? …. Nothing. No feeling, no rush, no less cramping, no improvement, nothing. But I had been told to expect that – remember it takes time for the new wire to take effect in the GPi.
 Thus began a ‘waiting game‘ of me coming in about once per month, and my neurologist and Boston rep changing the stimulation areas and/or increasing the stimulation amount, while looking for that ‘sweet spot‘. The GPi, since it’s bigger than the STN, can handle more stimulation – on my STN side I don’t think I ever got above 4.0 on the mA (milliamp) scale; in the GPi, I’m told, we can go to 6.0 and possibly higher!
Thus began a ‘waiting game‘ of me coming in about once per month, and my neurologist and Boston rep changing the stimulation areas and/or increasing the stimulation amount, while looking for that ‘sweet spot‘. The GPi, since it’s bigger than the STN, can handle more stimulation – on my STN side I don’t think I ever got above 4.0 on the mA (milliamp) scale; in the GPi, I’m told, we can go to 6.0 and possibly higher!
But after six months, I was starting to get a little nervous… We were increasing the stimulation, trying different areas, pulse rates, etc., with the end result still being no change to the dystonia. We had started out top most contacts, figuring they would be the place to start. But now the seventh month began… and I was downright depressed. By now I should feel at least something, you’d think?
 So we continued with the monthly changes.Then, in April of this year, the FDA approved a new product from my good friends at Boston Technologies – what they call their new Vercise Neural Navigator with STIMVIEW XT™! This new visualization software works with their Cartesia™ directional lead (which I have), and allow your doctor to see in real-time the location of leads, or electrodes, along with the accompanying brain structures, within the brain of a Parkinson’s patient! I can’t explain all that goes into this, but I think an example will help.
So we continued with the monthly changes.Then, in April of this year, the FDA approved a new product from my good friends at Boston Technologies – what they call their new Vercise Neural Navigator with STIMVIEW XT™! This new visualization software works with their Cartesia™ directional lead (which I have), and allow your doctor to see in real-time the location of leads, or electrodes, along with the accompanying brain structures, within the brain of a Parkinson’s patient! I can’t explain all that goes into this, but I think an example will help.
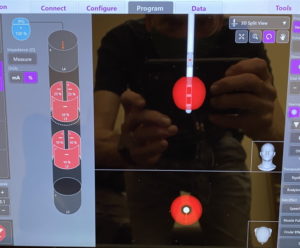
This is a picture of my GPi area using the old software. Note that it really only shows the lead and the size of the field – no idea as to where it’s located in the GPi, nor the size and shape of adjoining brain structures:
Now compare that to the NEW Vercise Neural Navigator images of my GPi:
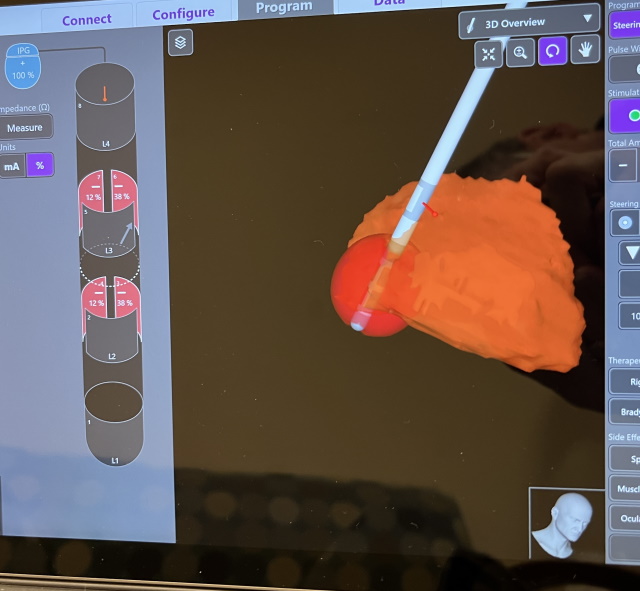
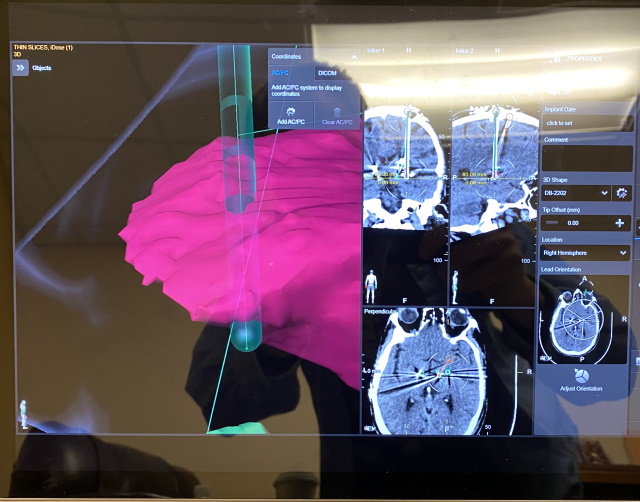
It is a very COOL thing to see! Those images are a near EXACT visualization of the shape of my GPi (down to the pixel); and also the exact location of the lead inside the GPi! But the sweet thing about it is that as they make changes to my program, we can see exactly how the shape and size of the stimulation area changes as it happens! In addition, this whole image can be viewed 360 degrees around; even some of the nearby brain structures can be shown – thus helping us know if the electrical field might be ‘leaking‘ into those other structures and causing side effects! No, I don’t work for nor am paid by Boston Scientific to serve as a spokesperson <grin>, but after using and seeing their tech I believe they are really at the top of the DBS arena!
Anyway, after viewing the lead placement via the Neural Navigator, we found we may not have been at the best location on the lead to deliver the appropriate stimulation; so we ended up moving the stimulation area down the lead a bit; they also rotated it around the lead so that the majority of the stimulation was into the GPi and not the surrounding areas. Then, once again, we waited.
 And… that brings us up to now… I would have liked to be able to say, “No more cramping toes!! Ya-HOOO!“; But unfortunately, that is not the case. As of yet, I am not feeling very much, if any, of the described benefits that GPi DBS is supposed to provide. My dyskenesias are still like they were before; and although I do feel that some of the rigidity in my legs does improve when the GPi is on, it’s not a big “WOW” event. But most importantly, my toes are still cramping up – I feel as much as they did before the GPi surgery! Now that doesn’t mean I’ve lost all hope and given up… yet… on this new GPi lead. My Boston rep, who’s been in the business a long time, said that with a lot of his patients/customers with dystonia, they would begin to see some changes in symptoms at the 1 year mark after surgery. But it would then take another year – i.e. at the 2-year mark after surgery – when they would have the full benefits and no longer need to do the monthly tuning process I’ve went through so far. I’m about 1.5 years into it, so the 2-year mark is coming up in May 2023…. and I’m starting to wonder. Just this last week, I was once again at my neurologist, where we decided to try the deepest contact on the GPi lead… Although it seemed to help a bit while I was there, that “improvement” began to wane after I went home. So, I keep hoping that, in time, we find that ‘sweet spot‘ along my GPi lead where the stimulation will FINALLY ‘take‘ and the dystonia in my toes will be reduced or GONE completely!
And… that brings us up to now… I would have liked to be able to say, “No more cramping toes!! Ya-HOOO!“; But unfortunately, that is not the case. As of yet, I am not feeling very much, if any, of the described benefits that GPi DBS is supposed to provide. My dyskenesias are still like they were before; and although I do feel that some of the rigidity in my legs does improve when the GPi is on, it’s not a big “WOW” event. But most importantly, my toes are still cramping up – I feel as much as they did before the GPi surgery! Now that doesn’t mean I’ve lost all hope and given up… yet… on this new GPi lead. My Boston rep, who’s been in the business a long time, said that with a lot of his patients/customers with dystonia, they would begin to see some changes in symptoms at the 1 year mark after surgery. But it would then take another year – i.e. at the 2-year mark after surgery – when they would have the full benefits and no longer need to do the monthly tuning process I’ve went through so far. I’m about 1.5 years into it, so the 2-year mark is coming up in May 2023…. and I’m starting to wonder. Just this last week, I was once again at my neurologist, where we decided to try the deepest contact on the GPi lead… Although it seemed to help a bit while I was there, that “improvement” began to wane after I went home. So, I keep hoping that, in time, we find that ‘sweet spot‘ along my GPi lead where the stimulation will FINALLY ‘take‘ and the dystonia in my toes will be reduced or GONE completely!
 (At this point you may ask, “But what if it doesn’t?” Well, I try not not to go there… But if that turns out to be the case… Yes, I will be EXTREMELY disappointed, having gone through all the expense, time, hardware, and pain of having the GPi installed. I know I’d rather be spending the time I have left concentrating on managing my disease as a whole, instead of constantly dealing day in and day out with this infernal toe cramping!! But what can I do about it? I guess I’ll look back on it and say I gave it a shot; but then I may have to look at other means – maybe drastic – to relieve or at least let me live with this dystonia.)
(At this point you may ask, “But what if it doesn’t?” Well, I try not not to go there… But if that turns out to be the case… Yes, I will be EXTREMELY disappointed, having gone through all the expense, time, hardware, and pain of having the GPi installed. I know I’d rather be spending the time I have left concentrating on managing my disease as a whole, instead of constantly dealing day in and day out with this infernal toe cramping!! But what can I do about it? I guess I’ll look back on it and say I gave it a shot; but then I may have to look at other means – maybe drastic – to relieve or at least let me live with this dystonia.)
 Well, I’m going to bring an end to this LONG tale I’ve told about the GPi – and also this series of posts. I may publish a short follow-up if and when we ever get this thing to work, thus finally ridding me of my dystonia symptoms…. but in any event, I hope that I’ve given you some knowledge about DBS, brain function, and Parkinson’s itself, that may help you cope or deal better with the disease.
Well, I’m going to bring an end to this LONG tale I’ve told about the GPi – and also this series of posts. I may publish a short follow-up if and when we ever get this thing to work, thus finally ridding me of my dystonia symptoms…. but in any event, I hope that I’ve given you some knowledge about DBS, brain function, and Parkinson’s itself, that may help you cope or deal better with the disease.
Again being a mind reader <wink>, I’m guessing you may be thinking about asking me if I still would have gone through DBS in the first place? The answer to that is a big YES – I’ve actually turned off my STN lead; and when I do… well let’s just say there is a BIG difference, so much so that I usually have to turn it back on within 30-60 seconds; so I know that lead does work and is helped me. We’ll just have to wait on the GPi lead and hope!
Thanks once again for reading Deep Brain Thoughts… I’ll be back soon with another post(s) that I’m working on. So stay tuned!
![]()



That was very educational and well written, Tom. Thanks for sharing your story. Joe and I are rooting for you and hoping the toe problem begins s to improve.