 Sleep Primer 101
Sleep Primer 101
What is Sleep?
“A condition of body and mind such as that which typically recurs for several hours every night, in which the nervous system is relatively inactive, the eyes closed, the postural muscles relaxed, and consciousness practically suspended.“
What’s the purpose of sleep?
 The stages of Sleep
The stages of Sleep
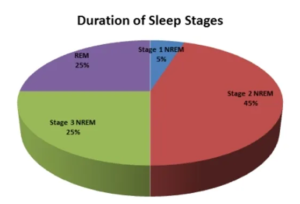
- First is Stage 1 (referred to as N1). This stage of sleep is the beginning of going to sleep – the transition between being awake and asleep. You are drowsy yet aware of things going on around you and you can be easily awakened from this stage.
- Next is Stage 2 (N2). Your heart rate and breathing slow down, and most importantly your body’s core temperature drops. Along with this your muscle activity decreases – you are now ready for the next stage!
- Stage 3 (N3). This is the ‘Deep Sleep‘ stage, where your brain and body get the most benefits of sleep. During this time your heart rate, breathing, and core body temperature are at their lowest. Also, the body repairs itself, regrows tissues, builds bone and muscles, and strengthens your immune system during this phase.
 Finally, there is REM sleep, or Rapid Eye Movement. This is when you dream – your eyes move rapidly, and heart/breathing rate increase. Also, for most folks, your body is ‘paralyzed‘ (called Sleep Atonia) during this time, so that you don’t ‘act out‘ your dream (which I am sure your spouse/partner is happy about!) It is also believed that this is the time when the brain is processing all of your memories from the day, figuring out what memories get ‘deleted‘, and what memories get moved from ‘short-term‘ storage to ‘long-term‘ storage. So the next time you have that dream of being naked while riding a Pogo stick through the stadium in the middle of a football game, it’s really just your brain figuring out what to do with your daily memories!
Finally, there is REM sleep, or Rapid Eye Movement. This is when you dream – your eyes move rapidly, and heart/breathing rate increase. Also, for most folks, your body is ‘paralyzed‘ (called Sleep Atonia) during this time, so that you don’t ‘act out‘ your dream (which I am sure your spouse/partner is happy about!) It is also believed that this is the time when the brain is processing all of your memories from the day, figuring out what memories get ‘deleted‘, and what memories get moved from ‘short-term‘ storage to ‘long-term‘ storage. So the next time you have that dream of being naked while riding a Pogo stick through the stadium in the middle of a football game, it’s really just your brain figuring out what to do with your daily memories! Your ‘Body Clock’
Your ‘Body Clock’
How Much Sleep Do We Need?
This is a very open-ended question, because it really depends on the individual. Our sleep needs changes as we get older, and are affected by health issues (such as Parkinson’s). But in general, it is believed that adults should have around 7-8 hours of sleep each night. Boy, if only we in today’s society could get that much sleep! Getting too little sleep results in what they call a ‘sleep deficit’ – if we don’t ‘repay’ this deficit, we can suffer the effects such as daytime sleepiness, cognitive issues, impaired reaction time, and the like. We’ll discuss more about this in regard to Parkinson’s – i.e. Sleep ‘Quality’ vs. ‘Hours Slept’.
 Sleep Disorders with Parkinson’s
Sleep Disorders with Parkinson’s
 Insomnia
Insomnia
 So what causes insomnia? There are a boatload of non-PD reasons why you might get insomnia (anxiety, depression, worry, etc.) but let’s instead concentrate on the reasons why we Parkies can get insomnia:
So what causes insomnia? There are a boatload of non-PD reasons why you might get insomnia (anxiety, depression, worry, etc.) but let’s instead concentrate on the reasons why we Parkies can get insomnia:- Meds – Believe it or not, some of the drugs we take to treat our motor symptoms can themselves cause insomnia! This is particularly true of dopaminergic drugs like MAO-B inhibitors and amantadine – these drugs have alerting properties and can make insomnia even worse.
- PD Motor Symptoms – Things such as rigidity and tremor can return during the night and affect your sleep. Trust me, it’s hard to get to sleep and stay asleep if your muscles are rigid or you get excessive tremors while in bed!
- Anxiety/Depression – These mood disorders can lead to difficulties falling asleep. If you are worrying all night about something (like what you need to get your wife the next morning because you forgot her birthday!!) it’s almost impossible for your mind to settle down enough to sleep.
- RLS/Sleep Apnea – Restless Leg Syndrome (RLS) and Sleep Apnea (disordered breathing) can cause anyone to have problems with sleeping; then adding Parkinson’s into this mix makes it even more difficult to get to and stay asleep.
- Progression of Disease – It’s sad to say that as our disease progresses the chances of us having sleep issues increases – this is simply the result of disease getting worse over time.
 Also, a lot of us worry about not getting enough sleep when we should also consider sleep quality. Is it any better to get 10 hours of sleep for instance, yet 1/2 of that time we are tossing and turning? I think not – we have to also consider the quality of the sleep we are getting. In addition, some folks may be able to get by with only 5 hours of sleep IF that sleep is mostly spent in deep or REM sleep. It really depends on the individual – some can get by with less, some with more. For me, I always would prefer to get quality sleep, as I think my brain benefits from that more than being able to sleep in till 10am each day! So just don’t consider your time but also your quality of sleep.
Also, a lot of us worry about not getting enough sleep when we should also consider sleep quality. Is it any better to get 10 hours of sleep for instance, yet 1/2 of that time we are tossing and turning? I think not – we have to also consider the quality of the sleep we are getting. In addition, some folks may be able to get by with only 5 hours of sleep IF that sleep is mostly spent in deep or REM sleep. It really depends on the individual – some can get by with less, some with more. For me, I always would prefer to get quality sleep, as I think my brain benefits from that more than being able to sleep in till 10am each day! So just don’t consider your time but also your quality of sleep. REM Sleep Behavior Disorder (RBD)
REM Sleep Behavior Disorder (RBD)
 I did some research and there hasn’t really been a lot of studies done on this and therefore not a lot of treatment options. Obviously, preventing significant injury is the first line of treatment – so it’s important to take safety measures to avoid accidents in the bedroom. This may include those involved sleeping in different beds or other sleeping arrangements; or implementing some type of ‘bar‘ or separation device between sleep partners. There are a few drugs that may help with this, such as Clonazepam and/or Melatonin – but there can be side effects with these so make sure you get approval from your neurologist before taking any of these! In any case, if this is occurring then we most defiantly need to contact our neurologist and discuss this with them. If you are using the ‘team‘ approach to your Parkinson’s care then most likely you also have a physiologist or psychiatrist on your team, and they can be a great source of help. Don’t be afraid to bring this
I did some research and there hasn’t really been a lot of studies done on this and therefore not a lot of treatment options. Obviously, preventing significant injury is the first line of treatment – so it’s important to take safety measures to avoid accidents in the bedroom. This may include those involved sleeping in different beds or other sleeping arrangements; or implementing some type of ‘bar‘ or separation device between sleep partners. There are a few drugs that may help with this, such as Clonazepam and/or Melatonin – but there can be side effects with these so make sure you get approval from your neurologist before taking any of these! In any case, if this is occurring then we most defiantly need to contact our neurologist and discuss this with them. If you are using the ‘team‘ approach to your Parkinson’s care then most likely you also have a physiologist or psychiatrist on your team, and they can be a great source of help. Don’t be afraid to bring this  Excessive Daytime Sleepiness (EDS)
Excessive Daytime Sleepiness (EDS)
 Treatments can involve limiting caffeine, improving sleep hygiene, light therapy, and minimizing drugs that may aggravate this condition (such as dopamine agonists). And sometimes EDS itself is a direct result of having insomnia and not getting enough sleep. Again, your neurologist and/or team can help, so if you experience this issue bring it up and discuss it at your next visit!
Treatments can involve limiting caffeine, improving sleep hygiene, light therapy, and minimizing drugs that may aggravate this condition (such as dopamine agonists). And sometimes EDS itself is a direct result of having insomnia and not getting enough sleep. Again, your neurologist and/or team can help, so if you experience this issue bring it up and discuss it at your next visit! My Experiences with Sleep Disorders
My Experiences with Sleep Disorders
 So I have a lot of experience with these sleep issues; in fact, this is one of the reasons why I have done so much research on sleep – remember, I’m the type of individual (otherwise known as an egghead!) who completely researches a topic that affects me so that I can gain a better insight into what it is and how to manage it. I wouldn’t call myself an ‘expert‘ on sleep by far, but it’s been something I have been investigating for many years. In any case, I have firsthand experience on how aggravating and debilitating these sleep issues can be. Not only on the physical side, but on the mental side as well. (Boy could I tell you a couple of stories on that! But I digress…) I’ve experienced most of these issues; including full-on insomnia (where I spent many a night with virtually NO sleep!); EDS, where during my last year of working I would fall asleep at my desk almost every day; and now I am having the lovely issue of falling asleep quickly but waking up early in the morning and not being able to go back to sleep! I’ve luckily not experienced too much of the sleep behavior disorder – although there have been a few times where I have acted out a dream – luckily with no damage to my wife (!); but I know this may mean that RBD could be in my future at some point (Oh joy!) So I know what anyone out there experiencing sleep issues feels like; and I, like you, am still trying to find a way to manage my sleep better – and I’ve tried a lot of things so far. Things that worked before my PD diagnosis simply don’t work as well now if at all.
So I have a lot of experience with these sleep issues; in fact, this is one of the reasons why I have done so much research on sleep – remember, I’m the type of individual (otherwise known as an egghead!) who completely researches a topic that affects me so that I can gain a better insight into what it is and how to manage it. I wouldn’t call myself an ‘expert‘ on sleep by far, but it’s been something I have been investigating for many years. In any case, I have firsthand experience on how aggravating and debilitating these sleep issues can be. Not only on the physical side, but on the mental side as well. (Boy could I tell you a couple of stories on that! But I digress…) I’ve experienced most of these issues; including full-on insomnia (where I spent many a night with virtually NO sleep!); EDS, where during my last year of working I would fall asleep at my desk almost every day; and now I am having the lovely issue of falling asleep quickly but waking up early in the morning and not being able to go back to sleep! I’ve luckily not experienced too much of the sleep behavior disorder – although there have been a few times where I have acted out a dream – luckily with no damage to my wife (!); but I know this may mean that RBD could be in my future at some point (Oh joy!) So I know what anyone out there experiencing sleep issues feels like; and I, like you, am still trying to find a way to manage my sleep better – and I’ve tried a lot of things so far. Things that worked before my PD diagnosis simply don’t work as well now if at all.Well, I think that is enough on the sleep subject. Hopefully I have helped all of you out there to know a little bit more about sleep; and encouraged you to not keep this ‘illegitimate child‘ of Parkinson’s hidden but rather bring it forward and discuss it – only then can we hope to get treatment for these disorders, and finally (hopefully) start getting a good nights sleep!